News
What’s to know about flat feet?
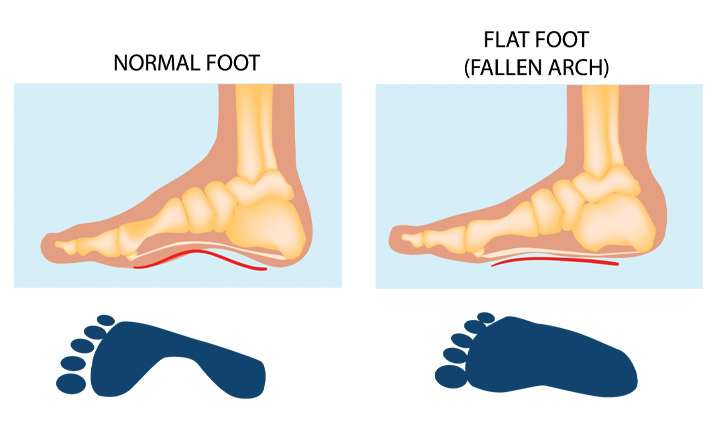
People with flat feet, also known as fallen arches, have either no arch in their feet or one that is very low.
There is usually a gap beneath the inner part of the foot when a person stands, as the arch raises off the ground slightly.
Flat feet only need treatment if they cause discomfort, indicate an underlying disorder, or lead to pain elsewhere in the body. Some people appear to have a very low arch or no arch without ever experiencing problems.
When flat feet do cause symptoms, simple devices and exercises can help to minimize the discomfort.
Read on to learn more about the causes, symptoms, and treatment of flat feet.

People with flat feet have a very low arch or no arch, meaning that one or both of their feet may be flat on the ground.
A human foot has 33 joints, which hold 26 different bones together. It also has over 100 muscles, tendons, and ligaments.
The arches provide a spring to the step and help to distribute body weight across the feet and legs. The structure of the arches determines how a person walks. The arches need to be both sturdy and flexible to adapt to stress and a variety of surfaces.
When people have flat feet, their feet may roll to the inner side when they are standing and walking. This is known as overpronation, and it may also cause the feet to point outward.
Many people with flat feet have no symptoms, but others will experience a variety of symptoms that generally depend on the severity of the condition.
Symptoms
The most common symptom of flat feet is pain in the feet. This can occur as a result of strained muscles and connecting ligaments.
Abnormal stresses on the knee and hip may result in pain in these joints. These stresses are likely if the ankles turn inward.
Pain most commonly affects the following parts of the body:
inside ankle, alongside possible swelling
- arch of the foot
- calf
- knee
- hip
- lower back
- lower legs
One or both feet may also feel stiff.
Flat feet can also cause an uneven distribution of body weight. This may result in shoes wearing down unevenly or more quickly than usual, especially on one side, which can lead to further injuries.
Causes
Common causes of flat feet include:
- genetic factors, as flat feet can pass from parents to children in the genes
- weak arches, meaning that the arch is visible when a person sits but the foot flattens onto the ground when they stand
- foot or ankle injury
- arthritis or rheumatoid arthritis
- damage, dysfunction, or rupture of the posterior tibial tendon
- nervous system or muscle diseases, such as cerebral palsy, muscular dystrophy, or spina bifida
Another condition that might cause flat feet is tarsal coalition. This condition causes the bones of the foot to fuse together unusually, resulting in stiff and flat feet.
Pediatricians usually diagnose this condition during childhood.
People are more likely to develop flat feet if they have obesity or diabetes. Flat feet are also more common during pregnancy.
Flat feet can develop with age too. Daily use of the feet can cause the posterior tibial tendon to weaken. This tendon is the primary support structure for the foot arch.
The tendon can become inflamed, called tendonitis, or tear after overuse. Damage to the tendon may cause the foot arch to flatten.
Flat feet can also occur as a result of a developmental fault that occurs during childhood or that develops with age or after pregnancy.

Children and infants may often appear to have flat feet.
In fact, the arch is usually present but still forming. In time, the arch should develop normally. The extra fat on an infant’s foot may hide the arch.
Having feet that appear flat during early childhood does not mean that a person will always have flat feet.
However, if a child has flat feet as a result of incorrect bone development or another condition, such as spina bifida, a doctor will often need to treat the underlying cause.
People with flat feet who do not experience pain or other symptoms do not usually need to consult a doctor.
However, anyone with the following symptoms should seek medical advice:
- flat feet that have only developed recently.
- pain in the feet, ankles, or lower limbs.
- symptoms that do not improve with supportive, well-fitted shoes.
- one or both feet becoming more flat
- the feet feeling rigid, stiff, heavy, and unwieldy
Most qualified healthcare professionals can diagnose fallen arches by examining the feet and observing the individual as they stand and walk.
The doctor will inspect the feet from the front and back. The individual may need to stand on the tips of their toes to allow the doctor to examine the shape and function of each foot.
A doctor will also look at the person’s medical history. In some cases, they may order an X-ray, CT scan, or MRI scan.
A podiatrist or physical therapist may recommend specific exercises to manage the symptoms of flat feet or prevent them from developing.
The American Academy of Orthopaedic Surgeons (AAOS) recommends the following exercises to improve strength and flexibility in the feet and ankles, which may help to relieve symptoms.
Heel cord stretching
A tight Achilles tendon will encourage the foot to roll inward. The aim of heel cord stretching is to stretch the Achilles tendon and posterior calf muscles.
- Stand facing a wall and place one hand on the wall at eye level.
- Place the leg that needs stretching approximately one step behind the other leg, and plant the heel firmly on the ground.
- Bend the knee of the front leg until you feel a stretch in the back leg.
- Hold for 30 seconds and then rest for 30 seconds. Repeat nine more times.
- It is essential to avoid arching the back and to keep it straight.
Perform this exercise twice a day.
The golf ball roll
This exercise requires a chair and a golf ball.
Sit on the chair with your feet firmly on the ground. Place the golf ball under the foot, and roll it forward and back under the arch of the foot for 2 minutes to stretch the plantar fascia ligament.
Some people with flat feet may automatically align their limbs in a way that prevents symptoms. People who are not experiencing symptoms do not usually require treatment.
If flat feet are causing pain, then supportive, well-fitted shoes can help. Extra-wide-fitting shoes can provide relief.
Fitted insoles and orthotics or custom-designed arch supports may relieve pressure on the arch and reduce pain if the feet roll too far inward. However, these products only treat the symptoms and do not provide long-lasting benefits.
People with posterior tibial tendonitis might also benefit from inserting a wedge into their footwear along the inside edge of the orthotic. This should relieve some of the load that the body places on the tendon tissue.
Wearing an ankle brace may also be beneficial until the inflammation reduces.
Doctors may advise some people to rest until their symptoms improve and to avoid activities that might aggravate the foot or feet.
A person with arthritis or a ruptured tendon might find that a combination of an insole and pain relievers can minimize their symptoms. If these do not work, surgery may be necessary.
Some bones do not develop properly in childhood, which can result in flat feet from birth continuing into adulthood. In these rare cases, surgical intervention may be necessary to separate fused bones.
When obesity is the cause of flat feet, losing weight might improve the symptoms.

People with other foot, ankle, or lower leg problems may find that flat feet can contribute to them or make symptoms worse.
Examples include:
- Achilles tendonitis
- arthritis in the ankle or ankles
- arthritis in the foot or feet
- bunions
- hammertoes
- plantar fasciitis, an inflammation of the ligaments in the soles of the feet
- posterior tibial tendonitis
- shin splints
Flat feet can affect the alignment of the body when a person is standing, walking, or running. As a result, they can increase the likelihood of pain developing in the hips, knees, and ankles.